Abstract
Background: There is little prospective, longitudinal data on the health outcomes of low count MBL in the U.S. adult population. We screened for MBL in asymptomatic adults with normal blood counts using highly sensitive flow-cytometry in a clinic-based cohort of participants from the Mayo Clinic Biobank and explored the relationship between MBL and risk of hospitalization with infection.
Methods: The Mayo Clinic Biobank is a large scale biorepository of 50,000 adults (age>18) seen in primary care-based clinics. All consented participants completed a health history questionnaire and provided blood samples. For the present study, we focused on the study participants from Olmsted County, Minnesota, 40 years of age or older who had stored PBMC. We used these PBMC to screen for MBL using an 8 color (CD38, CD45, Kappa, Lambda, CD19, CD23, CD5 and CD20) flow cytometry assay validated to consistently detect clonal B-cell events to the 0.005% level (1/20,000 events). The sensitivity of this approach of collecting 500,000 events from isolated PBMC is 2-3-fold higher than collecting 500,000 events from whole blood due to the increased concentration of lymphocytes in these samples.
Infections associated with hospitalization were considered serious or life-threatening infections. Every hospitalization at both Mayo Clinic and Olmsted Medical Center hospitals in Olmsted County, MN following the sample collection was reviewed to document hospitalization with infection. Data on hospitalization with infection was abstracted from clinical records using our previously published approach (Moriera, Leukemia 27:136). This approach allows medical record validation and review of detailed clinical and treatment information related to infection. For this analysis, follow-up began at date of sample collection and ended at the earliest of death, migration from Olmsted County, or 12/31/2016. The individual abstracting information on hospitalization for infection was blinded to the results of MBL screening.
Chi-square tests were used to assess associations between MBL status and demographic characteristics. Cox regression models were used to determine association with risk of hospitalization with infection accounting for the competing risk of death using Fine Gray models.
Results: We screened for MBL in 1045 Olmsted County residents age 40 and older. Of these, 984 (94%) had interpretable results. 119 of these 984 (12%) had a clonal B-cell population detected including 106 (11%) with CLL phenotype (CD5, CD19, CD20 [dim], CD23, kappa or lambda light chain restriction [dim]).This analysis focused on the 106 individuals with CLL-like MBL clones (mean age 69 years, 55% male) and the 865 individuals with normal immunophenotype (mean age 61 years, 40% male).
The presence of CLL phenotype MBL was strongly associated with age. MBL was detected in 3% of patients age 40-49 years, 7% of those 50-59, 10% of those 60-69, 20% of those 70-79, and 27% of those age 80+ (p<0.001). MBL was also more common among men (women 8%; men 14%; p=0.003).
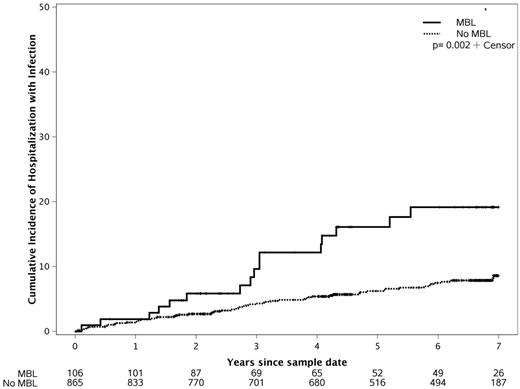
After a median follow-up of 7 years from biobank enrollment, 76 of the 971 participants were hospitalized with infection in Olmsted County at least once. The estimated cumulative incidence of infections at 7 years was 19% for LC MBL and 9% for those without MBL (Figure). The most frequent site of infections for which these individuals were first hospitalized were pneumonia (14 individuals; 18%), cellulitis (20 individuals; 26%), urinary tract infection (21 individuals; 26%), and blood stream infection (6 individuals; 8%). An association between LC MBL and hospitalization with infection was observed with the unadjusted HR for hospitalization with infection among the 106 Olmsted County residents with LC MBL relative to the 865 Olmsted County residents with normal immunophenotype is 2.41 (95%CI: 1.39-4.19; p=0.002). After adjusting for age and sex, the HR is 1.65 (95% CI: 0.95-2.88; p=0.08).
Conclusions:
We report one of the first studies to systematically explore the relationship between LC MBL and the risk of serious infection. It appears that individuals with LC MBL may be at increased risk for serious infection. If this observation is confirmed, it would suggest that 5-10% of adults over age 40 (6-12 million U.S. adults) have a largely unstudied condition with potentially serious health implications.
Shanafelt: Hospira: Research Funding; AbbVie: Research Funding; Celgene: Research Funding; Pharmacyclics: Research Funding; Jannsen: Research Funding; GlaxoSmithKline: Research Funding; Genentech: Research Funding. Kay: Gilead: Research Funding; Agios: Membership on an entity's Board of Directors or advisory committees; Pharmacyclics: Research Funding; Tolero Corporation: Research Funding. Parikh: Pharmacyclics: Research Funding; AstraZeneca: Honoraria; Pharmacyclics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal